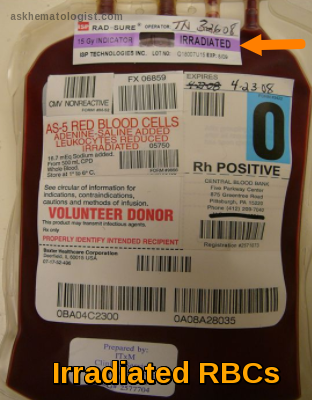
What’s this irradiation label on this bag?!!!

Immunohematology Made Easy (2)
General Topics – Key Principles and Everyday Practices
📘 Available now in PDF & EPUB formats
🔗 Visit Store

(This conversation is happening in the blood bank, next to the blood component fridge. 'T' is closely inspecting an RBCs bag.)
Characters:
Immunohematology Made Easy (2)
General Topics – Key Principles and Everyday Practices
📘 Available now in PDF & EPUB formats
🔗 Visit Store
- 'S': Someone who has been working in the blood bank for a while.
- 'T': Someone who just started working in the blood bank.
T: Hey, 'S', I keep seeing these bags with the "IRRADIATED" sticker on them. I understand that something was done to the bag, but why do only certain bags need this? And what exactly does it mean for the blood?
S: Excellent question, 'T'! This is a very important safety step that we perform for specific patients. Let’s break it down step by step.
Blood irradiation simply means exposing cellular blood components—such as RBCs, Platelets, and Granulocytes—to a controlled and calculated dose of radiation, usually using gamma rays or X-rays.
T: Radiation? That sounds serious! Why do we do this?
S: Exactly! Don’t just do things blindly—try to understand the reason behind them!
This irradiation is an additional step we apply to blood components for a very important reason. What is it?
It’s to prevent something called:
Transfusion-Associated Graft-versus-Host Disease (TA-GVHD).
T: Graft-versus-Host… like what happens in transplants? Can that happen from just a regular blood transfusion?
S: Yes, exactly the same concept! Though thankfully, it’s quite rare. Blood components contain immune cells from the donor, specifically T lymphocytes.
In TA-GVHD, these donor T cells recognize the patient’s body as foreign and start attacking it. Normally, the patient’s immune system can handle these donor cells, but problems arise when:
- The patient’s immune system is very weak and unable to fight back (due to certain diseases or treatments).
- The patient is on immunosuppressive drugs.
- The donor is a relative of the patient or the bag is HLA-matched. In this case, the patient’s body may not recognize the donor’s cells as foreign, allowing them to survive and proliferate, but at the same time, these donor cells attack the patient’s body.
T: Got it, that makes sense. So, irradiation stops these T cells from attacking?
S: Exactly! Radiation damages the DNA of the T cells, preventing them from multiplying or launching an attack. This effectively neutralizes the risk of TA-GVHD.
T: So, who exactly needs irradiated blood?
S: Patients with weakened immune systems, as we just discussed. The key groups include:
- Patients receiving intrauterine transfusions (before birth).
- Premature infants or low-birthweight newborns.
- Patients with congenital immunodeficiencies.
- Those undergoing stem cell or bone marrow transplants.
- Patients with certain cancers or those on strong immunosuppressive drugs (e.g., Fludarabine).
- Patients receiving granulocyte transfusions.
- Anyone receiving blood from a relative or an HLA-matched donor.
T: Understood. So how is irradiation done in practice?
S: We place the blood bag in a specialized device called a blood irradiator, which delivers a precise dose:
- U.S. standards: At least 25 Gy at the center of the bag and 15 Gy at any other part.
- European standards: Minimum of 25 Gy anywhere in the bag, but the allowed range can go up to 50 Gy.
This dose destroys the T cells.
We also use indicator labels that change color to confirm the bag has been irradiated, and the machines are regularly checked to ensure they deliver the exact required dose.
T: Does irradiation affect the blood itself? Like its quality or how long we can store it (shelf life)?
S: Good point! Yes, it does have some effects, especially on Red Blood Cells (RBCs).
Irradiation causes slight damage to the RBC membrane, leading to increased potassium leakage and some cell breakdown during storage. Because of this, the shelf life of the blood bag may change. This is why we follow strict guidelines, typically based on:
- American (AABB) guidelines.
- European guidelines.
- But most importantly, the policy of your specific institution.
Shelf Life Rules for RBCs:
-
American Standards:
- Irradiation can be done at any time before the bag’s original expiration date.
- The new expiration date becomes: 28 days from the irradiation date OR the original expiration date, whichever comes first.
Example:
- An RBC bag has an original shelf life of 42 days. If irradiated on Day 10, the new expiration date will be Day 38 (10 + 28) since that’s earlier than Day 42.
- If irradiated on Day 20, adding 28 days would bring it to Day 48, which exceeds the original Day 42 expiration, so the bag will still expire on Day 42.
-
European Standards:
- Irradiation must be done within the first 28 days from donation (older bags cannot be irradiated).
- The new expiration date becomes: 14 days from irradiation OR 28 days from donation, whichever comes first.
Example:
- If a bag is irradiated on Day 10, it will expire on Day 24 (10 + 14) since that’s earlier than Day 28 from donation.
- If irradiated on Day 20, adding 14 days brings it to Day 34, but since that’s past Day 28, the bag still expires on Day 28.
T: Wow, that’s really precise! So the expiration date must be carefully checked after irradiation.
S: Absolutely! Ideally, we try to irradiate RBCs as close to transfusion as possible.
If an irradiated RBC bag isn’t transfused within ~24 hours, it’s often recommended to wash the bag before giving it to the patient. This is mainly to remove excess potassium that may have leaked.
T: What about platelets? Does their shelf life decrease too?
S: Luckily, no. Platelets tolerate irradiation much better.
They can be irradiated at any point within their shelf life and still keep their original expiration date.
T: One last question?
S: Ask away, my friend!
T: Doesn’t leukoreduction also prevent GVHD?
S: That’s a common question! Leukoreduction significantly reduces the number of white blood cells, but it doesn’t eliminate them completely. Some T cells may still remain in amounts that can cause TA-GVHD in high-risk patients.
That’s why leukoreduction is NOT considered a replacement for irradiation when the goal is to prevent TA-GVHD.
However, some newer pathogen inactivation technologies treat blood components to reduce infection risks, and these methods also disable T lymphocytes.
So, blood components that undergo pathogen reduction often don’t require irradiation to prevent TA-GVHD.
T: This is super useful, 'S'! Now that I understand why we irradiate blood and how it affects storage, everything is much clearer. It’s clearly a critical step for patient safety.
S: Exactly! It’s all about protecting patients with weakened immune systems.
And always keep asking questions, 'T'—that’s the best way to learn in the blood bank!
Immunohematology Made Easy (2)
General Topics – Key Principles and Everyday Practices
📘 Available now in PDF & EPUB formats
🔗 Visit Store
📘 New to Blood Bank?
Start your 5-day journey with Immunohematology Made Easy — a simple, beginner-friendly guide with real-life examples!
👉 Get Your Copy Now